Medicare and Medicaid are facing a familiar quandary: how to provide coverage for new weight loss drugs with price tags that could effectively bankrupt the federal government’s health care budget while simultaneously ensuring continuous coverage for all other health care services used by millions of Americans.
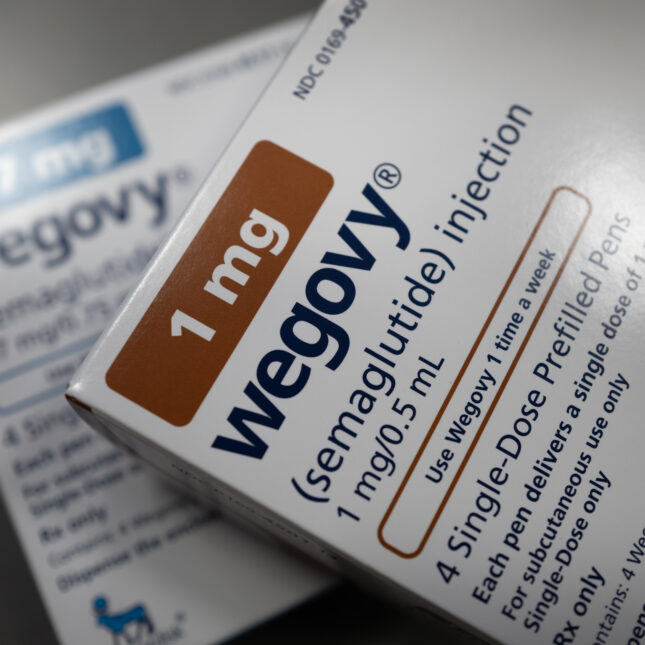
The Centers for Medicare and Medicaid Services announced in March 2024 that it would cover Wegovy (semaglutide), a new and expensive weight loss medication, for beneficiaries with cardiovascular disease and obesity. Efforts by the U.S. House of Representatives could nudge CMS to cover it more broadly for people with obesity alone.
That would have a huge cost impact. Wegovy’s current list price in the United States is $1,349 per month. Medicare spending on this class of drugs, called GLP-1s, has increased from $57 million in 2018 to $5.7 billion in 2022, while Medicaid spending for these drugs increased from $383 million to $1.8 billion in that time period. A report by the Senate Committee on Health, Education, Labor, and Pensions (HELP) estimates that treating even half of Medicare and Medicaid beneficiaries with obesity would cost $166 billion per year, nearly the cost of total spending on all prescription drugs in 2022 ($175 billion).
This article is exclusive to STAT+ subscribers
Unlock this article — plus in-depth analysis, newsletters, premium events, and networking platform access.
Already have an account? Log in
Already have an account? Log in
To submit a correction request, please visit our Contact Us page.











STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect