
Bird flu snapshot: This is the latest installment in a series of regular updates on H5N1 avian flu that STAT is publishing on Monday mornings. To read future updates you can also subscribe to STAT’s Morning Rounds newsletter.
When pathologist Thijs Kuiken looks at what’s happening in the U.S. response to the H5N1 bird flu outbreak in dairy cows, he’s reminded of a difficult period in the Netherlands, where he lives, back in the late aughts.
Large goat and sheep farms in the country were hit with outbreaks of what is known as Q fever every year from 2007 to 2010. The disease, caused by the bacterium Coxiella burnetii, primarily affects ruminants — sheep, goats, and cows. But people can contract it too. Some don’t get sick. Some have flu-like illness and recover. But some develop chronic Q fever syndrome, a debilitating condition. Hundreds of people in the Netherlands still suffer from the condition as a consequence of the 2007-2010 epidemics.
H5N1 is a virus that scientists fear might one day trigger a pandemic; Q fever is a bacterial disease that when present in an environment can lead to significant numbers of infections in people. But the similarity Kuiken sees is how, in both cases, the initial inclination is to treat these events in animals as an economic problem for the agricultural sector, rather than as an agricultural problem that could have large human health consequences as well.
“My overall concern about this outbreak is that it’s being treated too much as an economic problem and too little as a public health and an animal health problem,” said Kuiken, who works in the department of viroscience at Erasmus Medical Center in Rotterdam.
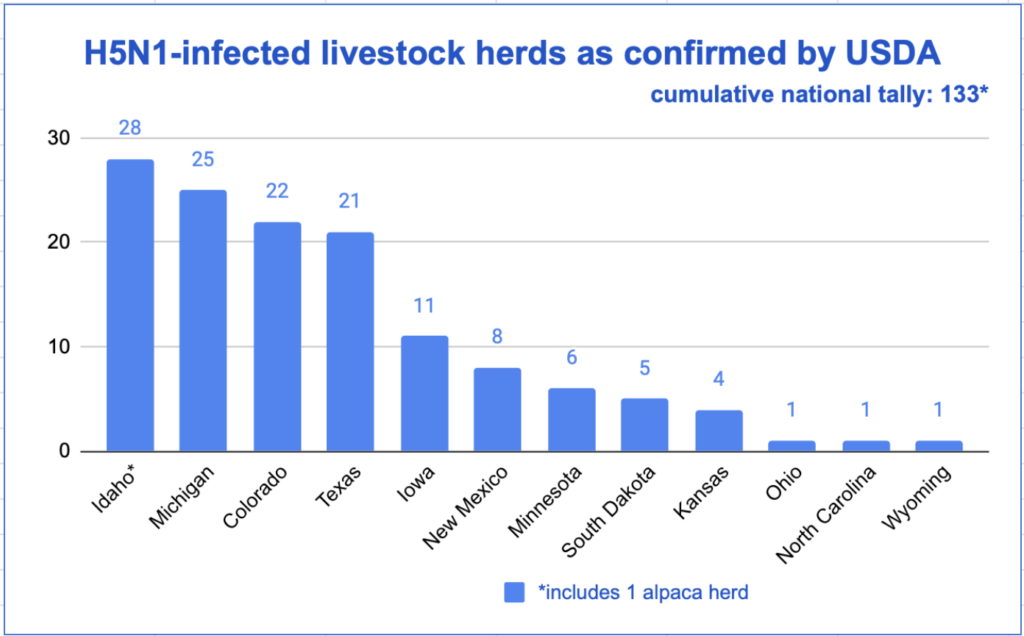
Kuiken is one of the influenza experts STAT spoke to for an article last week analyzing the response to the H5N1 outbreak in cows to date. He and others worry about the lack of urgency in the U.S. response and the apparent absence of a comprehensive plan for driving the virus out of cattle. Agriculture Secretary Tom Vilsack believes the answer is better biosecurity on farms. But with the number of affected farms continuing to rise — the figure hit 139 in 12 states at the end of last week and those are the farms where farmers actually allowed testing to take place — there is no sense that the tide is turning. (The USDA’s count was 133 on Friday, which did not include the two latest detections in Iowa and four newest in Colorado.)
Letting H5N1 become established in cows would give the virus a chance to adapt to a mammalian species, increasing the risk it would acquire mutations that would help it become capable of spreading to and among people.
The response to the Q fever outbreaks was similar, Kuiken said: “At the beginning it was treated mainly as an economic problem and a problem of the dairy goat sector and was dealt with by the ministry of agriculture.”
Infected animals shed large amounts of the bacteria in their milk, urine, feces, and placentas; the infections induced “abortion storms” on farms with pregnant animals, Kuiken said. The bacteria wafted off the farms in the wind. “There were people who would cycle by these farms and become infected.” But the locations of affected farms were not publicly disclosed, for privacy reasons. (Sound familiar?) “So even if people were concerned that they might get infected and wanted to keep away from these areas, they did not know where they were,” he said.
Eventually the country’s health minister stepped in to demand that the outbreaks be treated also as a human health problem. “It really was an important lesson for the veterinary and medical authorities,” Kuiken said.
At present in the H5N1 outbreak, control over the response lies firmly in the hands of the U.S. Department of Agriculture. Though there have been numerous reports of sick farmworkers — many more than the three who have tested positive for H5N1 in this outbreak to date — few have been tested. The Centers for Disease Control and Prevention reported Friday that at least 53 people have been tested for the virus since the outbreak was first detected. That figure was 51 at the end of the week before last.
Efforts to try to get a handle on how many people may have been infected have been stymied because in many cases farmers have refused to allow public health workers on their properties to talk to and test their workers. But finally, there’s been a breakthrough on this front: Health authorities in Michigan are conducting a small serology study, with the cooperation of an undisclosed number of farms in that state. Participating workers are filling in questionnaires describing their encounters with cows and their daily duties, and are giving a blood sample that will be analyzed for antibodies to the virus. The CDC is collaborating with Michigan on the study.
Another study that is getting underway is part two of a Food and Drug Administration effort to assess the risk H5N1 virus poses to commercial milk production. In early May the agency reported that of nearly 300 store-bought milk samples, about 1 in 5 contained fragments of bird flu viruses, but the viruses had been killed by pasteurization. (The FDA and USDA released a preprint — a study that hasn’t yet gone through peer review — on Friday showing that commercial pasteurization techniques reduce virus in milk to undetectable levels.)
Part two of the milk study will focus on some milk products the first iteration didn’t test, Don Prater, the FDA’s acting director of the Center for Food Safety and Applied Nutrition, told journalists last week. They include: cream cheese, aged raw milk cheese, butter, and ice cream. Results are some weeks off, he said.
Coming sooner — today, in fact — USDA will start taking applications for an assistance plan to compensate farmers for lost income due to reduced milk production in H5N1-infected cows. With money to cover losses actually on the table, it’s hoped farmers will finally see a reason to test animals they suspect are infected with the virus.
To submit a correction request, please visit our Contact Us page.











STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect