Untreated vision loss and high LDL cholesterol have been added as two new potentially modifiable risk factors for dementia in a report released Wednesday by the Lancet Commission.
These new additions join 12 other risk factors outlined by the commission, affiliated with University College London, in previous reports on dementia prevention, intervention, and care in 2017 and 2020. The other risk factors are lack of education, hypertension, physical inactivity, diabetes, social isolation, excessive alcohol consumption, air pollution, smoking, obesity, traumatic brain injury, and depression.
The commission’s latest findings suggest more ways of preventing dementia than previously known, according to Gill Livingston, a professor of psychiatry at University College London and co-author on the report.
“A lot of surveys have asked people of 50 and above what illnesses they most are concerned about, and dementia tends to come up as the highest one,” Livingston said. “And yet there’s really quite a lot that we can do to change the scales and make it less likely.”
Avoidable vision loss and blindness are estimated to affect 12.6% of adults aged 50 and older. By conducting a meta-analysis of 14 cohort studies, the commission found a 47% increase in risk for dementia in adults who have untreated vision loss. In another meta-analysis, cataracts and diabetic retinopathy had significant associations with dementia risk.
Follow-up studies in the U.S. found that those who had cataract extractions had significantly reduced risk for dementia — a 29% decrease — opposed to those who did not have cataract extractions. Cataracts are marked by the lens of the eye becoming cloudy, resulting in hazy vision. They can arise with aging and other conditions that cause proteins in the lens to break down and clump together.
Livingston said the role of vision loss as a risk factor for dementia can be compared to the loss of hearing, identified as a risk factor in a previous report.
“One of the ways in which both vision and hearing act is in terms of cognitive stimulation,” Livingston said. “People who have hearing loss have a reduction in the volume of the temporal lobe.”
Maya Koronyo-Hamaoui, a professor of neurosurgery at Cedars-Sinai Medical Center, said the retina is a significant aspect of the link to dementia. It’s the only central nervous system tissue that’s both connected directly to the brain and not shielded by bone, allowing for noninvasive and high-resolution imaging.
“In our cohorts, when we see damage to the retina, there’s almost always the same extent of damage in the brain,” Koronyo-Hamaoui said of her own research.
Molecular changes in the retina affect processes like circadian rhythms — responsible for regulating the sleep-wake cycle — and vision, which Koronyo-Hamaoui believes could potentially mirror damage in the brain.
There’s a social aspect of vision loss that plays into dementia risk, Livingston said.
“People who have these losses go out less, see other people less, are much more likely to become socially isolated,” Livingston said. The report notes that vision loss most often goes untreated in low-income and middle-income countries.
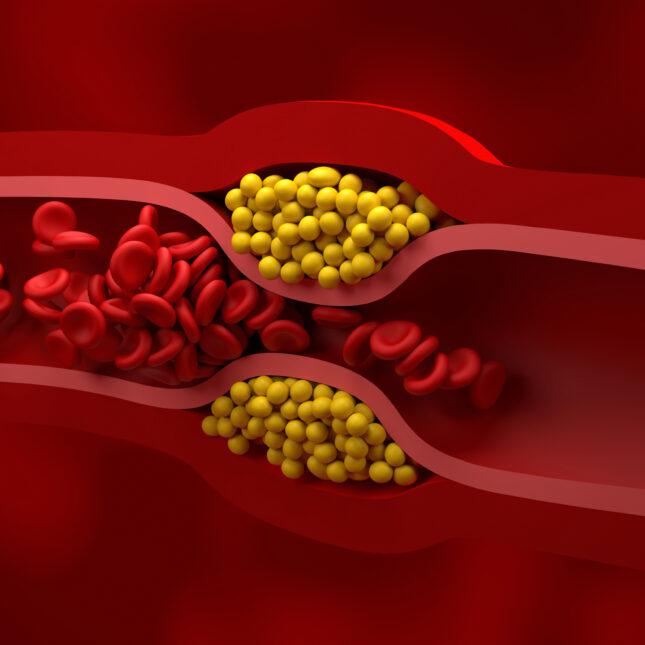
Higher LDL cholesterol — also known as the “bad” cholesterol — was also associated with higher incidence of dementia, the report’s authors found. High total cholesterol and low HDL were also found to be risk factors for dementia in an analysis of 27 studies. LDL is the type of cholesterol responsible for buildup and blockage of arteries, while HDL removes LDL from the bloodstream and carries it back to the liver.
The commission said that individuals with high LDL specifically in midlife, ages 18 to 65, would be at highest risk for dementia.
What’s behind the association between high cholesterol and dementia risk? “Excess brain cholesterol is associated with people having higher amyloid within their brain and also with increased stroke risk,” Livingston explained. Buildup of the sticky protein amyloid is associated with Alzheimer’s, while increased stroke risk is associated with vascular dementia.
Erin Ferguson, a Ph.D. student and researcher in the department of epidemiology and biostatistics at the University of California, San Francisco, described the research as “very exciting work” because of the prevalence of high cholesterol and statin use in older adults. But she said that the current evidence citing LDL as a risk factor is variable, drawing on what she’s seen in her research at Kaiser Permanente looking at vascular comorbidities of dementia.
“Even looking at ages 55 to 65 in this cohort, I’m not able to see an association between high LDL cholesterol and dementia risk,” Ferguson said of her own research cohort. “I’m a little surprised that LDL was the main cholesterol listed when there’s a whole lot of other evidence showing that HDL may play a factor.” She added that triglycerides, a type of fat that circulates in the blood and stores energy, may also play a role in preventing dementia.
Regulating levels of cholesterol, like lowering LDL, also decreases the chance of cardiovascular events like stroke and heart attack, Ferguson noted. These events, in turn, are risk factors for dementia, namely vascular dementia.
There are several ways to maintain normal cholesterol levels to mitigate dementia risk. The go-to for older adults are statins, according to Ferguson. For younger adults, she suggests exercise and diet to keep LDL levels in check.
This story has been corrected to reflect that the retina is the only central nervous tissue that is both connected to the brain and not shielded by bone.
To submit a correction request, please visit our Contact Us page.











STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect